Introduction
Do you want answers to your questions of badder prolapse or cystocele ? I have answers to all your questions such as is bladder prolapse curable? If so how? and is it dangerous? What will happen if I do not get any treatment? Can it be fixed with Physical therapy? What is surgery like? Will I need surgery? These and many more will be answered as you read this blog post.
Prevalence
This is the most common of the 3 kinds of organ prolapse seen in associated with urinary incontinence seen in the older female population 60 years and older.
Anatomy
The 3 main functions of the pelvic floor are
- Bladder
- Bowel
- Sexual function
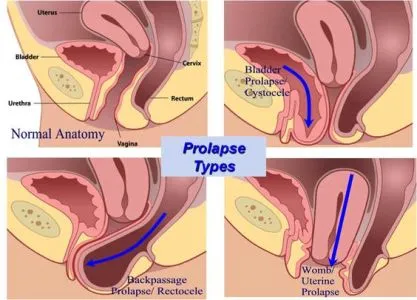
The associated organ systems of the above listed functions are located in the pelvic floor. The bladder, the rectum and the uterus are supported by tissues called the ligaments.Most of the time, these organs are held in place by a combination of strong ligament and pelvic floor muscles.When the supportive ligaments and muscles get weak the organs start slide from their places to bulge through the vagina.When there is a bladder prolapse the bladder starts to protrude through the front ( anterior ) vaginal opening.
Degrees of Bladder Prolapse : The degree of prolapse is measured in the extent of prolapse relative to the hymen.
- 1st degree
- 2nd degree
- 3rd degree
Symptoms of Bladder Prolapse:
- Urinary Incontinence-
- Stress Incontinence : urinary leakage with coughing sneezing and laughing
- Urge Incontinence : Decreased ability to control and subside the urge to urinate is felt.
- Incomplete bladder emptying
- Recurrent urinary tract infections
- Difficulty inserting a tampon and difficulty with keeping the tampon in during menstruation. Common patient statements are “ the tampon doesn’t stay inside for long or I have trouble inserting the tampon.“
- Difficulty initiating the urine steam.
- A feeling of bladder fullness which increases as the end of the day usually feels better when patient is laying down .
- A bulge can be seen and felt at the vaginal opening. Can be seen during straining/ coughing in lying down and seen and felt in standing as well (in severe cases).
- Pain and discomfort with intercourse.

Causes /Risk Factors of Bladder prolapse
- Childbirth( Vaginal delivery , especially instrument assisted )
- Constipation
- Chronic coughing as in C.O.P.D.( lung diseases)
- Repetitive heavy lifting and strenuous exercises such as crossfit
- Postmenopausal. Estrogen is responsible to keep the vaginal tissues supple and in good tone hence post menopause the tissues (ligaments ) loose elasticity and are prone to bladder prolapse.
- Any pelvic Surgery
- Genetic factors
- Caucasian Ethnicity

Diagnosis of Bladder Prolapse
- A Through History and Physical Exam to assess the degree of prolapse
- Test for Bladder prolapse :
- Urodynamics : to know the type of incontinence.
- Urine test to check for UTI ( urinary tract infection )

Treatment for Bladder prolapse
- The treatment depends on the degree of prolapse.
- No treatment may be required if it’s not interfering with your daily activities or causing urinary issues.
- Prolapse can remain asymptomatic until the organ descent has reached a certain point and hence it may not be recognized until advanced. In some women the prolapse progresses rapidly and some it remains stable for years .Handa et al ( 2004 ) found that spontaneous regression was seen in cases of mild prolapse.
- Miedel et al (2011) found that only small % of women with POP worsen over 5 years.
- Bladder prolapse is not dangerous in mild cases. It’s an inconvenience interfering with daily activities and in most of the less severe degrees of prolapse can be treated effectively with a combination of lifestyle change, pelvic floor therapy and medications.The severe degree of prolapse may require surgery.
1. Lifestyle changes :
- Wt. loss ( if overweight )
- Treating Chronic Cough
- Avoiding straining and managing constipation
- Pelvic floor muscle exercises Kegel exercises
- Pessary .May require some practice to insert the Pessary.May require regular follow up with Dr .
A. Pelvic Floor Exercises :
A,PFMT ( Pelvic floor muscle training ) has been concluded to have a positive effect on POP (pelvic organ prolapse ) due to the following hypothesized reasons (Bo, 2004)
- Women learn to contract the pelvic floor before and with any increase in the intra abdominal pressure , such as bearing down when lifting heavy wts .
- Regular strengthening exercises build up the strength of the Pelvic floor and the structural support overtime .
B. The Knack
- The Knack is a technique that we pelvic PT’s call instruction to consciously contract the PFM before an activity that requires an increase in the intra abdominal pressure for eg lifting something heavy or before a cough or a sneeze (if you can predict it).
- I instruct my patients “ Squeeze before you sneeze “.
- This will take some practise but will prove to be effective, as reported by my patients about 3 to 4 weeks of regular pelvic floor exercises.

3. Medications:
Estrogen Replacement Therapy
4.Surgery
Surgical options may be considered as a means of treatment usually in severe degree of prolapse and when conservative management was not effective. Prolapse recurs in 70% of the women who had surgery.(Iglesia et al 2010) and 1/3rd of the operated women undergo one further surgical procedure for prolapse (Olsen et al 1997)
- Types of Surgery
- Reconstructive Surgery – restores organs to their original place.Normal activities can be resumed after recovery from surgery.
- Obliterative Surgery -which narrows and closes off the vaginal to support the prolapse, sexual intercourse is not possible after this surgery.
This can be done in one of the following ways.
Open Surgery
Laparoscopic Surgery
Robotic assisted surgery
Recovery time : Depends on the type of Surgery but the Dr usually recommends no heavy lifting, straining , and sexual activity for 6 weeks post surgery.

Conclusion
- Bladder prolapse is a treatable condition and patients can return to a good quality of life after the diagnosis of a bladder prolapse.
- Mild degrees of Prolapse, can be treated effectively and successful most of the time with Physical therapy , Pessary and lifestyle modification .
- Surgery is an option in advanced prolapse.

References :
Evidenced based Physical Therapy for Pelvic Floor 2nd edition

